The spine is a unique biokinematic system, it can bear loads without damage, but like all structures, it wears out over time. At a young age, the stable condition is maintained thanks to the rapid regeneration abilities, but after 50 years, their supply gradually fades, which leads to the development of osteochondrosis.
Osteochondrosis is the most common degenerative-dystrophic pathology of the spinal column, which, as it progresses, spreads to the nearby structures of the spinal segment.

Development theories
The etiology of osteochondrosis is unknown. Current theories of the development of the disease:
- Metabolic.Changes in the metabolism of the disc due to its drying out (at a young age, the amount of water is 88%, with age the water content decreases to 60%).
- It's worth it.Changes in spinal circulation (occurs in adulthood, but earlier development is possible due to injuries, metabolic disorders, infections).
These theories are sometimes combined into an involution based on a violation of trophism, especially in tissues that do not have blood vessels. In childhood, there is a network of blood vessels in the intervertebral discs, but after the complete development of the spine's architecture, this network is closed by connective tissue.
- Hormonal theorymore controversial. Hormonal status plays a certain role in the development of osteochondrosis, but it is inappropriate to refer only to hormone levels. This theory applies mostly to postmenopausal women.
- Mechanical theorytalks about the relationship between the occurrence of osteochondrosis and overloading of certain parts of the spine.
- Anomaly theory- isolated case from mechanical theory. Anomalies of the vertebral bodies, fusion of the bodies, fusion of the arch due to inadequate biomechanism stimulate the overload of the discs and cause the destruction of the bone tissue.
These theories have a right to exist, but none of them are universal. It is more correct to call osteochondrosis a multifactorial disease characterized by genetic predisposition and provoking factors.
Factors contributing to the development of the disease
- Gravity Factor:for the spine, any non-physiological movement is nothing more than a trigger for many muscle reactions.
- Dynamic factor:the greater and longer the load on the spine, the more and longer it is exposed to trauma (persons prone to long-term forced positions; constant lifting of heavy objects).
- Dysmetabolic factor:insufficient nutrition of the spinal column due to autoimmune disorders and toxic effects.
It is known that eating from aluminum dishes leads to its accumulation in the bones, which later contributes to the development of osteochondrosis. Eating foods made from aluminum and iron alloys has a harmful effect on the human body. When preparing food, microparticles enter the gastrointestinal tract, and since they also contain lead, this metal accumulates in the body, poisoning with which is manifested by neuroosteofibrosis (tissue changes at the junction of tendon and muscle).
- Genetic factor.Each person has an individual level of elasticity that directly correlates with the ratio of fibers (collagen and elastin) in the connective tissue and is genetically inherited. Despite the above, there are standards in the ratio of fibers, deviations lead to faster wear and tear of the spinal column.
- Biomechanical factor– non-physiological movements on the joint surface of the spine. This is caused by muscle atrophy (the clinical symptom is pain when bending and turning).
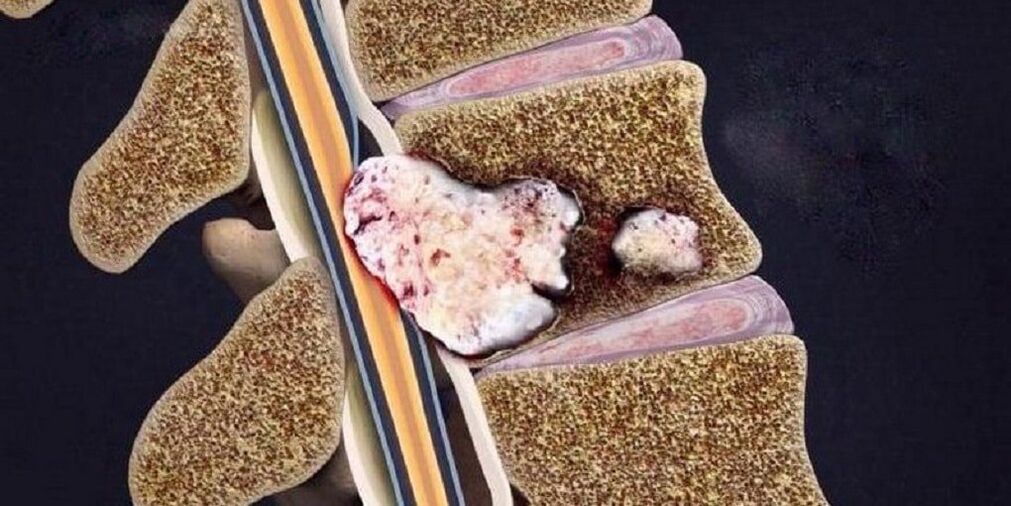
- Aseptic-inflammatory factor– most often a rapid inflammatory process in the intervertebral discs. Microdefects develop in the spinal disc due to malnutrition of the disc. Dead tissue areas are formed in these microdefects.
Symptoms of osteochondrosis of the spine
The main symptom of osteochondrosis is back pain, which can be constant or intermittent, painful or acute, most often aggravated by sudden movements and physical activity.
Osteochondrosis is a common disease among athletes. This is due to a mismatch between physiological capabilities and motor loads, which contributes to microtrauma and wear and tear of the spinal tissue.
The localization of the symptoms largely depends on the part of the spine in which the pathological process occurs (cervical, thoracic, lumbosacral). If the pathological process is localized in several parts, then this condition is called mixed osteochondrosis.
| Type of osteochondrosis | Cervical | Chest | Lumbosacral | Mixed |
|---|---|---|---|---|
| Clinical picture |
|
|
|
the pain is stable or extends to all parts of the spine. |
| Complications |
|
|
compression myelopathy (compression of the spinal cord by various neoplasms). |
all complications that are possible in cervical, thoracic, lumbosacral osteochondrosis. |

Stages of osteochondrosis
| Platoon | First | Second | Third | Fourth |
|---|---|---|---|---|
| Changes in the spine |
|
|
Rupture and displacement of the vertebral plate by immersion in the cavity of other surrounding elements, which causes the development of local symptoms of inflammation. | Destruction of other elements of the intervertebral articulation, abnormal arrangement of joint surfaces, marginal bone growths. |
| Patient complaints | It indicates a lack or discomfort when staying in the same position for a long time. | Discomfort and pain during certain types of exercise. | Pain in the back, neck, lower back, sacrum, or tailbone, depending on the location. | Constant pain in the whole spine. |
Differential diagnosis
- Acute myocardial infarction.The pain is concentrated in the area of the heart, and only from there it radiates (spreads) to the neck, lower jaw and arm. The disease begins for no reason or after physical activity, with the appearance of compression pain that is not related to the movement of the spine. After half an hour, the pain reaches its maximum, the person develops shortness of breath and fear of death. The diagnosis is confirmed by an electrocardiogram (ECG) and markers of myocardial necrosis.
- Subarachnoid hemorrhage(bleeding between the arachnoid and pia mater of the brain). In some cases, severe spinal pain can occur due to the toxic effect of spilled blood on the spinal roots. The main clinical symptom is the presence of blood in the cerebrospinal fluid.
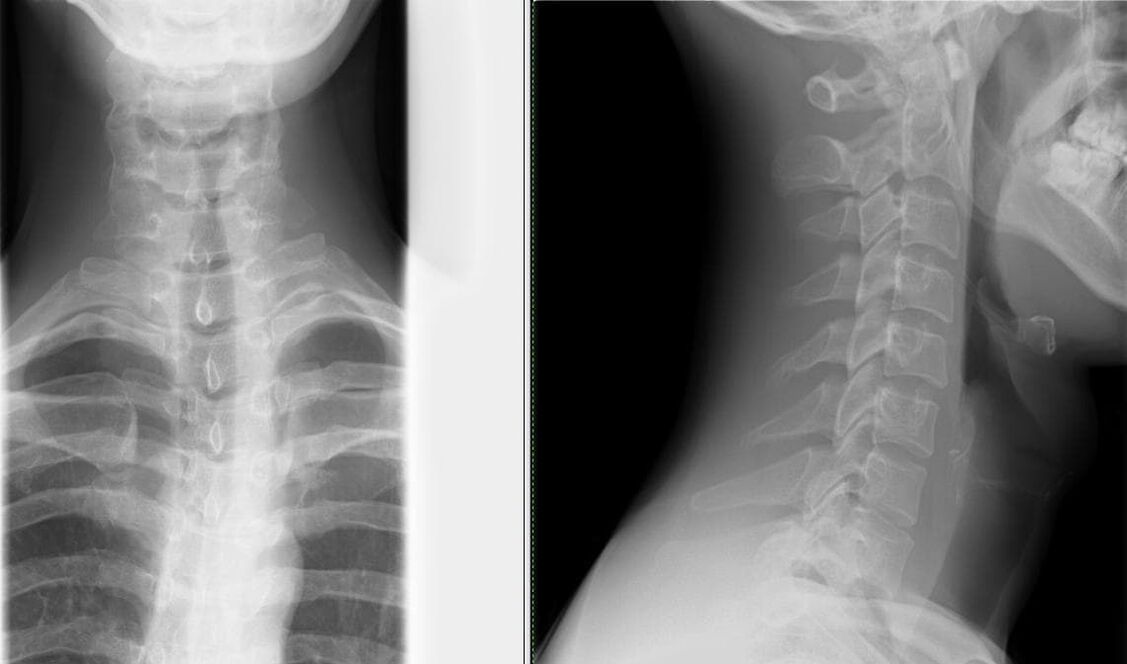
- Spine disorders.Minimal examination: X-ray of the skull and cervical spine in frontal and lateral views. The most common anomalies of the spine are the following: fusion of the atlas (the first cervical vertebra) with the occipital bone, intrusion of the edges of the occipital foramen into the cranial cavity, fusion of the vertebrae, changes in the shape and size of the vertebra. vertebrae.
- Cervical lymphadenitisit may also be accompanied by neck pain, which is sometimes aggravated by bending and turning. Establishing the diagnosis is not difficult: enlarged, painful lymph nodes; a frequent sore throat in the medical history.
- Multiple myeloma.Spinal pain appears gradually, against the background of progressive weight loss and intermittent fever. The main laboratory sign is protein in the urine.
- Tumor or metastases in the spine.Evidence for malignant tumors: progressive weight loss, laboratory changes, and ultrasound examination of the sources of metastasis - kidneys, lungs, stomach, thyroid gland, prostate.
- Rheumatic and infectious-allergic polyarthritisit is distinguished by medical history, moderately elevated body temperature, and predominant damage to large joints.
- Masked depression.Patients "force" non-existent pathologies (in this context, the symptoms of osteochondrosis), the attempt to explain to them the essence of what is happening runs into a wall of misunderstandings. Signs of disguised depression: decreased mood, concentration and performance; sleep and appetite disorders; suicidal thoughtsand actions.
- Gastric and duodenal ulcers, pancreatitis and cholecystitisIt is diagnosed by the correlation of pain with food intake and laboratory tests (FGDS, general blood test, biochemical blood test, activity of pancreatic enzymes, ultrasound examination of abdominal organs).
Diagnosis of osteochondrosis
- Most often, the patient turns to a neurologist, who collects an anamnesis about the patient's life and illness and performs a neurological examination. The neurologist examines the spine in three ways (standing, sitting and lying down). When examining the back, special attention should be paid to posture, the lower angles of the shoulder blades, the ridges of the hip bones, the position of the shoulder girdle, and the expression of the back muscles. Deformation, pain and muscle tension are determined during palpation.
- When establishing the diagnosis of osteochondrosis, additional consultation with specialists is required to rule out pathologies with similar symptoms (cardiologist, therapist, rheumatologist).
- Completion of mandatory laboratory tests (general blood test, general urine test, biochemical blood test).
- Confirmatory studies are useful:
X-ray of the spine in two views – the simplest method for identifying changes in the spinal column (narrowing of the gap between the vertebrae);Depending on the degree, different changes can be seen on X-rays:
Degree First Second Third Fourth X-ray signs No radiological sign. Changes in the height of the intervertebral discs. Protrusion (bulging into the spinal canal) or even prolapse (loss) of the intervertebral discs. Formation of osteophytes (marginal bone growths) at the contact point of the vertebrae. computed tomography (CT) and magnetic resonance imaging (MRI) - not only to identify changes in the spine, but also to determine the pathologies of other organs;USDG MAG (ultrasound dopplerography of the main arteries of the head) - an ultrasound examination of the circulatory system of the head and neck, which enables early diagnosis of the degree of changes in blood vessels.
What are the treatment methods for osteochondrosis?
Drug therapyit must be strictly individual and differentiated, the prescription of drugs is carried out by the doctor after the diagnosis.
The main drugs used in the treatment of osteochondrosis:
- Pain relief is provided by pain relievers and non-steroidal anti-inflammatory drugs (NSAIDs). NSAID treatment should be as short as possible, 5-7 days is enough to relieve pain. If the pain is poorly controlled and a constant dose of pain medication is required, you can take selective COX-2 inhibitors.
- Antispasmodics reduce pain and relieve muscle spasms.
- Transcutaneous pain relief method: ointment, the active ingredient of which is NSAID; anesthetic cream; use with anti-inflammatory and pain-relieving drugs; corticosteroids are added for greater effect.
- Treatments for the regeneration of an inflamed or compressed nerve and for improving blood microcirculation: B vitamins, neuroprotective agents, nicotinic acid.
- Oral chondroprotectors – glucosamine, chondroitin sulfate. With regular intake, they help stop destructive cartilage changes. Chondroprotectors are incorporated into the framework of the cartilage tissue, thereby increasing the formation of the bone matrix and reducing joint damage. The most favorable composition: chondroitin sulfate + glucosamine sulfate + glucosamine hydrochloride + non-steroidal anti-inflammatory drugs (NSAIDs). These drugs are called combined chondroprotectors.
Non-drug treatment methods:
Neuroorthopedic measures. An important point in the treatment of osteochondrosis is the observance of a rational physical activity regime. Lying in bed for a long time and minimal physical activity is not only not good for the spine, but also leads to a permanent symptom - back pain.Therapeutic exercise (physiotherapy) it is prescribed when the patient is in a satisfactory condition (especially during the period when the signs of the disease decrease), the main goal is to strengthen the muscle ligament.To prevent falls, to improve movement coordination and the functioning of the vestibular apparatus (in elderly patients), balancing plates, platforms and paths are used in gymnastics therapy.
Manual therapy with severe neck pain. It is prescribed with special vigilance and according to strict indications. The main goal is to eliminate the pathobiomechanical changes of the locomotor system. The main reason for prescribing manual therapy is the pathological tension of the paravertebral muscles. Do not forget about many contraindications to this type of treatment, which apply to osteochondrosis - massive osteophytes (abnormal growths on the surface of bone tissue) that develop in the fourth stage of the development of this pathology.Physiotherapy procedures in the acute period: - ultrasound;
- phonophoresis;
- ultraviolet radiation;
- impulsive currents;
- neuroelectrical stimulation.
Physiotherapy procedures in the subacute period: - electrophoresis;
- magnetotherapy.
Massage. A superficial, relaxing massage with rubbing elements is used in all types. As soon as the symptoms of pain are alleviated with the help of the massage, they smoothly move on to the more intense elements of rubbing. When learning the technique of acupressure (local) massage, this type is preferred.The issue of surgical interventions is decided strictly individually, depending on the indications and the patient's condition.

Preventive measures

- Competent selection of furniture (especially in the workplace). The work chair consists of a flat and solid backrest. The bed includes a medium firm mattress, a medium soft pillow (if possible, an orthopedic mattress and pillow).
- Vision, posture, bite correction.
- Reasonable selection of shoes (especially important for drivers). The maximum size of the heel is 5 cm.
- Wearing a restraint belt, bandage or corset while working.
- Movement correction: avoid bending and turning, lift weights with a straight back and legs bent at the knees.
- Change your position more often: don't stand or sit for a long time.
- Proper nutrition: limit the amount of sweet, salty, fatty, spicy foods. The most dangerous food for bones is white sugar, as it leaches calcium from bone tissue. The diet should include fruits, berries, vegetables, eggs, nuts, meat, kidney, liver, fish, legumes and dairy products.
- Protect yourself from sudden temperature changes, especially hot water in the bath, sauna, swimming pool, etc. is dangerous. , because it relaxes the back muscles, and in this condition even a small injury is not felt, but has tragic consequences for the spine and even the musculoskeletal system in general.
- Water treatment is not only preventive, but also therapeutic. Swimming combines stretching and relaxing the muscles.
- Treatment of chronic diseases.
- Active and regular vacation.
Examples of effective exercises for the prevention of cervical osteochondrosis that can be performed directly at the workplace:
- sitting on a chair, looking ahead. The brush covers and supports the lower jaw. Pushing the head forward and down through the resistance (tension phase); relax and stretch the neck muscles, slowly move your head back (relaxation phase);
- sitting on a chair, looking ahead. The right palm is on the right cheek. Slowly tilt your head to the left, try to touch your left shoulder with your ear, and stay in this position for 3-5 seconds. Left palm to the left cheek and do the same to the right shoulder;
- sitting on a chair, looking ahead. Your hands are on your knees. We tilt our head to the right, hold it for 5-7 seconds and very slowly return to the starting position. Then tilt your head to the left and do the same accordingly.
Conclusion
The high frequency and social importance of osteochondrosis determine the scientific interest in the problem. The disease affects not only the elderly, but also occurs more and more often among young people, which attracts the attention of neurologists, neurosurgeons, orthopedic traumatologists and other specialists. Timely diagnosis and appropriate treatment of this pathology ensures social adjustment and future quality of life.















































